The chemical structure of gabapentin (Neurontin) is derived by addition of a cyclohexyl group to the backbone of gamma-aminobutyric acid (GABA). Gabapentin prevents seizures in a wide variety of models in animals, including generalized tonic-clonic and partial seizures.
The exact mechanism of action with the GABA receptors is unknown; however, researchers know that gabapentin freely passes the blood-brain barrier and acts on neurotransmitters.
Gabapentin has a cyclohexyl group to the structure of neurotransmitter GABA as a chemical structure. Even though it has a similar structure to GABA, it does not bind to GABA receptors and does not influence the synthesis or uptake of GABA.
Gabapentin works by showing a high affinity for binding sites throughout the brain correspondent to the presence of the voltage-gated calcium channels, especially alpha-2-delta-1, which seems to inhibit the release of excitatory neurotransmitters in the presynaptic area which participate in epileptogenesis.
Even though there is no evidence for direct action at the serotonin, dopamine, benzodiazepine, or histamine receptors, research has shown gabapentin to increase total-blood levels of serotonin in healthy control subjects.
The elimination half-life of gabapentin is 5 to 7 hours, and it takes two days for the body to eliminate gabapentin from its system.
One benefit of gabapentin use is its mild side-effect profile. The most common side effects are fatigue, dizziness, and headache.
Gabapentin has no activity at GABAA or GABAB receptors of GABA uptake carriers of brain. Gabapentin interacts with a high-affinity binding site in brain membranes, which has recently been identified as an auxiliary subunit of voltage-sensitive Ca2+ channels. However, the functional correlate of gabapentin binding is unclear and remains under study.
Gabapentin crosses several lipid membrane barriers via system L amino acid transporters. In vitro, gabapentin modulates the action of the GABA synthetic enzyme, glutamic acid decarboxylase (GAD) and the glutamate synthesizing enzyme, branched-chain amino acid transaminase.
Results with human and rat brain NMR spectroscopy indicate that gabapentin increases GABA synthesis. Gabapentin increases non-synaptic GABA responses from neuronal tissues in vitro. In vitro, gabapentin reduces the release of several mono-amine neurotransmitters.
Gabapentin prevents pain responses in several animal models of hyperalgesia and prevents neuronal death in vitro and in vivo with models of the neurodegenerative disease amyotrophic lateral sclerosis (ALS). Gabapentin is also active in models that detect anxiolytic activity.
Although gabapentin may have several different pharmacological actions, it appears that modulation of GABA synthesis and glutamate synthesis may be important.
Is Gabapentin Addictive ?
Asking about the signs someone is addicted to gabapentin first begs the question: What is gabapentin?
To answer that question requires putting gabapentin in perspective as a pharmaceutical drug that, while providing relief to thousands of people for nerve pain, also has the potential for abuse. It isn’t an opioid, but it has found a niche audience among those who take it recreationally, and for doctors who began to seek alternatives to narcotics as the opioid epidemic reached its apex, it seemed like a safer alternative.
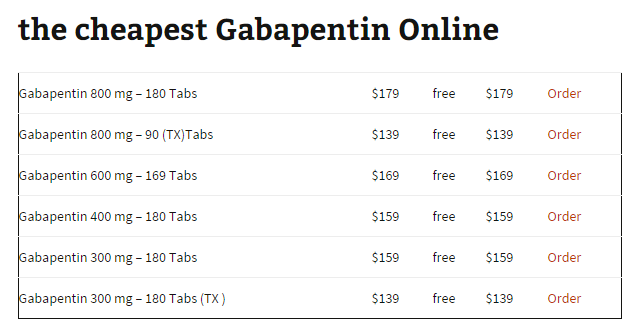
In 2016, gabapentin was the 10th most prescribed drug in the United States, with 64 million prescriptions written that year . That was up from 39 million prescriptions written only four years earlier, in large part because “gabapentin, an anticonvulsant and analgesic for postherpetic neuralgia, has been thought to have no abuse potential despite numerous published reports to the contrary,” according to a 2018 article in the journal Psychology of Addictive Behaviors.
In that particular article, researchers analyzed data from a study of drug users in Kentucky who reported using gabapentin for non-medical purposes. Their findings? “Overall, the sample reported having initiated gabapentin more than 10 years earlier after having it prescribed for a legitimate, though generally off-label, medical indication (e.g., pain, anxiety, opioid detoxification). Participants reported use of gabapentin in combination with buprenorphine, other opioids, cocaine, and caffeine to produce sought-after central nervous system effects (e.g., muscle relaxation, pain reduction, sleep induction, feeling drunk, and feeling ‘high’).”
Gabapentin, such studies reveal, can be problematic. Whether used in conjunction with other drugs or on its own, it can be abused, which makes it a substance of concern. To understand the signs someone is addicted to gabapentin, however, requires some knowledge of what it is, where it comes from, how it works and how it can be addictive.
Comparative Studies
Gabapentin and lamotrigine have been compared in an open, parallel-group, add-on, randomized study in 109 patients with uncontrolled partial epilepsy and learning disabilities. The two drugs were similarly efficacious, with similar incidences of adverse events and serious adverse events. Neither lamotrigine nor gabapentin exacerbated any of the challenging behaviors observed in these patients.
The most common adverse reaction to gabapentin was somnolence, which was mostly reported during the initial titration phase.
In a double-blind comparison of gabapentin and lamotrigine in 309 patients with new-onset partial or generalized seizures, the target doses were gabapentin 1800 mg/day and lamotrigine 150 mg/day.
Severe adverse events were reported in 11% of patients taking gabapentin and 9.3% of patients taking lamotrigine. Two patients had serious adverse events thought to be related to the study drug; one took an overdose of gabapentin and the other had convulsions with lamotrigine. The most frequent treatment-related adverse events in both treatment groups were dizziness, weakness, and headache; 11% of patients taking gabapentin and 15% of those taking lamotrigine withdrew because of adverse events. There was an increase of over 7% in body weight from baseline in 14% of the patients taking gabapentin and 6.6% of those taking lamotrigine. There were benign rashes in 4.4% of those taking gabapentin and 11% of those taking lamotrigine.
The hypothesis that both amitriptyline and gabapentin are more effective in relieving neuropathic pain than diphenhydramine has been tested in a randomized, double-blind, triple crossover, 8-week trial in 38 adults with spinal cord injuries [18]. Maximum daily doses were 2600 mg for gabapentin and 150 mg for amitriptyline.
Amitriptyline was more efficacious in relieving neuropathic pain than diphenhydramine. Withdrawal because of possible adverse reactions occurred five times during gabapentin treatment:
(1) shortness of breath;
(2) dizziness, fatigue, and nausea;
(3) increased spasticity and pain;
(4) fatigue, drowsiness, constipation, and dry mouth; and
(5) severe itching.
The four most frequent adverse events were dry mouth, drowsiness, fatigue, and constipation, which were all more common with amitriptyline.