Gabapentin is commonly used to treat some types of nerve pain but is classified as an anticonvulsant medicine, not as an opioid or painkiller.

Gabapentin was first approved in 1993 and is used to treat:
-
- postherpetic neuralgia, a nerve pain caused by the shingles virus (herpes zoster),
- restless legs syndrome (RLS), a painful movement disorder in the legs
- partial seizures in adults and children at least 3 years old who have epilepsy
Gabapentin works by affecting chemicals and nerves in the body that are involved in the cause of seizures and in some types of nerve pain.
Gabapentin is not a federally-controlled drug substance and does not contain an opioid (narcotic) medication. However, gabapentin misuse and abuse has been reported, and it may be restricted in some states through their state drug-monitoring program. Gabapentin abuse can boost the high a person gets from opioid painkillers, muscle relaxants, and anxiety medications. This can be dangerous and potentially life-threatening.
In 2019, the FDA issued an alert that serious breathing problems have been reported with gabapentin and other related drugs, like Lyrica (pregabalin) in people at risk of slowed breathing.
-
- This includes people who use opioid pain medicine or CNS depressants, people with chronic obstructive pulmonary disease (COPD, and the elderly.
- These serious breathing problems may be fatal.
- Read more about this serious FDA warning here.
Avoid or limit the use of alcohol (in beverages or medicines) with gabapentin as it can worsen drowsiness or dizziness. Ask you doctor about drinking alcohol while you are taking gabapentin.
What type of pain does gabapentin treat?
Gabapentin is approved by the FDA to treat:
Postherpetic neuralgia: nerve pain that can occur due to an outbreak of shingles. Shingles, also known as herpes zoster, occurs when the chicken pox virus deep-seated in your nerve activates again later in life and causes a serious skin rash. Not everyone gets postherpetic neuralgia from shingles, but it can be painful if you do. It causes a burning nerve pain that lasts for months, or even years, after the rash and blisters have cleared up.
Restless legs syndrome (RLS): an uncontrollable urge to move your legs around, often at night. This is usually due to leg discomfort. It may occur most often when you are sitting, laying down, or during bedtime. It can be disruptful to sleep and travel. It is thought RLS may occur due to an imbalance of the chemical dopamine in the brain.
Gabapentin has also been used off-label for the treatment of other types of neuropathic (nerve) pain like peripheral diabetic neuropathy, fibromyalgia and trigeminal neuralgia. “Off-label” uses of gabapentin are uses that have not been approved by the FDA and are not found in the package insert, but may have been accepted for use by healthcare providers based on clinical use.
How does gabapentin come?
There are several brand names of gabapentin including Gralise, Horizant, and Neurontin. Use only the brand and form of gabapentin your doctor has prescribed.
Gralise (gabapentin) is indicated for the management of postherpetic neuralgia only. It is not used for epilepsy. Gralise comes as a 300 and 600 milligram (mg) extended-release (ER) tablet and in a 30-day starter pack of 78 tablets. A generic option is not yet available.
Horizant (gabapentin enacarbil) is used in adults to treat either nerve pain due to postherpetic neuralgia (PHN) or restless legs syndrome (RLS). Horizont is also an extended-release 300 mg or 600 mg tablet and is not interchangeable with other gabapentin products. A generic option is not yet available.
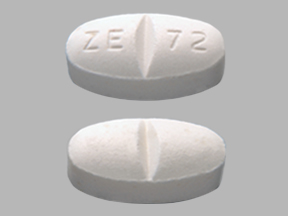
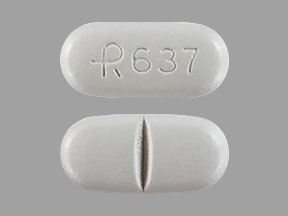
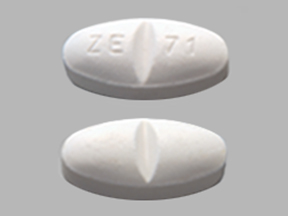
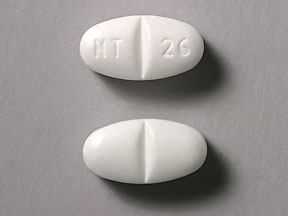
Neurontin (gabapentin) is an immediate-release form used to treat seizures in adults and children who are at least 3 years old, in addition to nerve pain due to shingles. It comes as 100, 300, or 400 mg oral capsules; 600 mg and 800 mg oral tablets, and as a 250 mg per 5 mL oral solution. It is also available as a generic option.
Some brands are only used for certain conditions, and these products may not be interchangeable. Check your medicine each time you get a refill to make sure you have received the correct form.
Some of these medicines may be expensive. Ask your healthcare provider if you are able to use a generic form of gabapentin for your condition (this may not always be possible). Generic options could save you hundreds of dollars each month, or may be less expensive than your insurance copay.
Also, check with the manufacturer who may offer copay cards or patient assistance programs to lessen your overall costs, if you qualify. Be sure to check for online coupons, too, that can save you money on both generics and brands.
To learn more about gabapentin, join the Drugs.com gabapentin Support Group and Q&A Section where you can ask questions, share experiences and keep up with the latest news.
This is not all the information you need to know about gabapentin for safe and effective use and does not take the place of talking to your doctor about your treatment. Review the full gabapentin information here, and discuss this information and any questions you have with your doctor or other health care provider.